BME Test – DO NOT USE
BME Department Senior Design Teams
 |
Senior Design 2020 – Biomedical Engineering Team 1  |
Team Sree Kolli |
Faculty Advisor(s) Yupeng Chen |
Sponsor ABB Sponsor Logo  |
bone model and hydrogel |
||||
Description Often times in the case of pediatric growth plate fractures, bone tissue will form within the growth plate, preventing normal growth from occurring. No method currently exists to prevent bone tissue formation, the only current solution being to remove the bony bridge after it has formed. The aim of this project is to develop an ex-vivo, 3D printed bone model that simulates various types of pediatric growth plate fractures and a biocompatible hydrogel that has the capability to seal therapeutic agents into this modeled fracture. The bone model and hydrogel will be utilized in the design of an injection system that can administer the treatment components directly to the injury site. These treatment components, janus-base nanotubes (JBNTs) encapsulating the protein-coding gene MATN3, promote the regeneration of cartilage tissue within the growth plate - preventing bone tissue formation and allowing normal growth to resume upon healing. This injection system offers a minimally invasive alternative for growth plate fracture healing. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 2  |
Team Nathan Friday |
Faculty Advisor(s) Martin Han |
Sponsor UConn Neural Prostheses Lab Sponsor Logo  |
|
|
||||
Description The main goal of this project is to construct an insertion device that will allow us to insert microelectrodes into the gray matter of the spinal cord that are connected to the bladder that patients no longer have control of. Our motivation for the completion of this project is primarily to enhance the daily lives of patients who suffer from spinal cord injuries and chronic pain all located to the lower appendicular of their body systems. The insertion device will utilize sensors which allow the operator to better understand the location of the implantation. This will take place through the use of a force and displacement sensor to measure the speed of the insertion and distance at which the microelectrode is implanted. We plan on utilizing SolidWorks and tissue design to create prototypes of our insertion design as well as a gelatin-agarose model of the spinal cord to test the device. We also used SolidWorks to design and prototype the device in order to test the compatibility with the holding frame, insertion rods, and force and displacement sensors. This prototype will then be used in conjunction with the instrumentation circuitry and the spinal cord model to test its performance and generate data for continuous improvement. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 3  |
Team Daniel Barry |
Faculty Advisor(s) Lakshmi Nair |
Sponsor UConn Health Sponsor Logo  |
|
|
||||
Description The goal of this project was to create an HPP-modified reacetylated glycol chitosan-based degradable hydrogel for localized drug delivery. This device allows the administration of drugs/molecules to specific sights in the body at a controlled rate through a degradation-mediated release. The HPP-modified reacetylated glycol chitosan-based hydrogel (HPP-GC) will be loaded with a payload during the cross-linking process, which is achieved using horseradish peroxidase (HRP) and hydrogen peroxide solutions. The HPP-GC is degradable by lysozyme, which is naturally occuring in the body. The degradation of the hydrogel is easily modified by its degree of reacetylation and the concentration of lysozyme coadministered with it. The payload can differ depending on the application at hand. The payload will be primarily released as the hydrogel degrades. The hydrogel will be completely degraded inside the body via lysozyme within a 2 week period. The hydrogel will be biocompatible and should have no adverse effects on the surrounding tissues. Thus far, a hydrogel has been designed that degrades within five days. A formal degradation study will be conducted to adjust this degradation rate. Furthermore, a drug release study will be conducted to observe the release of Curcumin from the hydrogel. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 4  |
Team Andrew Lioio |
Faculty Advisor(s) Patrick Kumavor |
Sponsor Defibtech, LLC. Sponsor Logo  |
|
|
||||
Description The purpose of this project is to create a mechanical model of the human thorax that will allow for benchtop testing of automated resuscitation devices which provide mechanical chest compressions (mCPR). Important properties that affect the motion of the human thorax are the elasticity constant and viscous damping coefficient. Current models used for testing only simulate the elasticity through the use of a linear spring. This new design adds pneumatic dampers in addition to the springs to add the element of nonlinearity. Sensors will also be integrated into the system to collect force and displacement data. This will provide real-time feedback on the chest compressions as well as information for a feedback system that can change the damping coefficient in real-time. The effectiveness of this model will be demonstrated by plotting its force-displacement data using mCPR devices and validating the data against clinical research of the physiological behavior of the human chest. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 5  |
Team Haining Li |
Faculty Advisor(s) Sabato Santaniello |
Sponsor NSEC Lab Sponsor Logo  |
|
|
||||
Description Psychogenic nonepileptic seizures (PNES) are a disease mainly caused by trauma, stress disor- ders, or depression. The symptoms of PNES are very similar to epileptic seizures, which usually lead to mis- diagnosing and thus result in ineffective treatments. These limitations can be refined by a relaxing EEG- based biofeedback system. This system contains a headset product to acquire and process EEG data in real-time and a new gaming app for Android plat- forms that positively reinforces the players based on the neural feedback provided by the EEG. The gaming part related to the subject’s reaction, and based on their performance, the application would change accordingly and hence, easing their stress. The design concept of our game is determined after a comprehensive searching on how to relax people. By using an EEG signal detector headset, we are able to obtain brainwaves from PNES patients and transform them into attention and meditation values. These inputs are crucial parameters for our game to be an EEG-based biofeedback system. The game will be changing its diffi- culty according to the user’s performance. Therefore, these feedback helps the player reduce their stress by providing ease when he/she is stressed. Constantly play- ing this game, patients can reduce the occurrence of PNES. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 6  |
Team Srinivas Setty |
Faculty Advisor(s) Sabato Santaniello |
Sponsor NSEC Lab Sponsor Logo  |
|
|
||||
Description Being the fourth most common neurological disorder in the United States, Epilepsy is a debilitating disease with widespread impact and dire side effects. By combining an amalgam of harrowing symptoms such as severe bouts of confusion, onset seizure, depression, and anxiety, epilepsy can transform even the simplest of tasks into agony. Therefore, the goal of this project is to provide clinicians with an automated framework for detecting the point of origination of seizures in the brain to assist with the bedside protocols of patients suffering from epilepsy. Using time series EEG data from 50 patients, this project seeks to develop machine learning based classification methods to detect anomalies in electrical activity in the brain, as these anomalies can often function as biomarkers for localized seizure activity. This will be done by using 18 different EEG signals from the 50 patients to develop metrics for anomalous detection through classification. Once the classification algorithms have been thoroughly tested and verified with testing data sets, a physical user interface mapping real time EEG data with the classification algorithms will be developed to function as a bedside decision support system for clinicians to seamlessly detect the origin of seizures. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 7  |
Team Renz Patrick Rebeca |
Faculty Advisor(s) Sabato Santaniello |
Sponsor NSEC Lab Sponsor Logo  |
|
|
||||
Description The purpose of this project is to develop a device capable of interpreting brain wave patterns from an electroencephalogram (EEG) in order to control the movements of an exoskeleton attached to the subjects hand. This project is focused on restoring the hand motion of stroke patients, though the system could be applied to a number of other motor disabilities such as paralysis. This device consists of two main parts, the EEG and the exoskeleton hand, which are interfaced using an Arduino. The EEG will provide raw brain wave data into the Arduino which will then be processed into more meaningful information that can be used to distinguish between different hand movements. The motors on the exoskeleton will then respond based on the information received from the Arduino causing the whole exoskeleton to move accordingly. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 8  |
Team Dylan Barlow |
Faculty Advisor(s) Syam Nukavarapu |
Sponsor TEST Lab Sponsor Logo  |
|
|
||||
Description Osteoarthritis is a chronic degenerative disease of articular joints and affects 50-60 million people in the US alone. Currently there are no proven effective treatments or therapies, which is largely attributed to the incongruence between in vitro and in vivo models used during testing. The excessive cost, timeframes, and ethical concerns of current testing processes all point to a need for improved methods, as well as a more accurate model of human in vivo conditions. Organ-on-a-chip devices aim to provide a more convenient and accurate way to replicate human conditions and study disease or pharmaceuticals. Although some organ-on-a-chip devices have been created thus far, a chip that models the synovial joint has yet to be designed. This project’s objective is to design and construct a synovial joint on a chip using CAD design and 3D printing. The chip is designed with three microchambers, one for bone, cartilage and synovium, respectively. Each channel has individual fluid flows, as well as cells seeded in hydrogel. We placed a common channel through the center of the chip to model vascularization as a means of introducing pharmaceutical therapies. Due to our focus and emphasis on accurately modeling in vivo conditions, the device created can rapidly increase the development and testing of osteoarthritis drugs and therapies. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 9  |
Team Emily Borges |
Faculty Advisor(s) Sangamesh Kumbar |
Sponsor UConn Health Sponsor Logo  |
|
|
||||
Description Using a critical sized long bone defect in rat models is a very common method of testing the efficacy of bone tissue engineering scaffolds. However, these scaffolds often lack the necessary mechanical properties to support bone regeneration. Therefore, a fixation device must be used to maintain the defect and provide support while the bone heals. Developing an external fixation device for rat femur models will allow for an accurate translation of additional bone healing factors (i.e. scaffolds and composites) onto larger scale models for use in future testing. Due to the average size of rat femurs and the traditional screw fixation method of external devices, bone fracture rates during implantation are a major problem in clinical and research settings. Developing a device to reduce the fracture rate will increase the effectiveness and efficiency of fixation devices and will allow for the study of other factors such as stiffness and load intensity. Using clamps, as opposed to the traditional screw fixation method, can mitigate bone fractures caused by screws. This project will explore the potential of a clamp fixation method in regards to bone fracture reduction while maintaining femur stability. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 10  |
Team Wissam Afyouni |
Faculty Advisor(s) Patrick Kumavor |
Sponsor R. Davids |
|
|
||||
Description The orthotic device designed, currently named the “Therawalk”, is a therapeutic walking assistant. The goal of the project is to create a versatile orthotic device that both aids patients in mobility and provides relief for arthritis. Therawalk incorporates a vibration component to help alleviate the pain caused by arthritis localized within the hands. This will benefit patients who need the aid of a cane, but find the use of one difficult due to the pain in their hands and who, as a result of this pain, struggle with maintaining grip on the cane handle. The cane handle was designed for optimal comfort and ease of use for patients with arthritis, with integrated functionality for the electrical components. Development of the Therawalk focuses primarily on the integration of electrical components such as the vibration motors and heart rate sensor to a mechanical cane design. Additionally, the cane design will be revisited to enhance aesthetic characteristics, and ensure optimal integration of the electrical components while leaving room for future improvements. The goal of this project is to produce a smart orthotic device that will help the patient's mobility in both clinical and home settings. The Therawalk will have components to deliver vibration therapy, as well as a flashlight and heart rate sensor. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 11  |
Team Matthew Chipdey |
Faculty Advisor(s) Patrick Kumavor |
Sponsor Biomedical Engineering Sponsor Logo  |
|
|
||||
Description One of the key components of our design is the software which makes it possible. As a proof of concept, we used MatLAB to process audio signals by transforming them into the frequency domain. These signals are processed onboard a laptop, and the main focus of the project is to refine this technology into smaller and more portable parts, with the ultimate goal of creating a system which can be mostly or completely contained inside the handle of the cane. At the time of writing, The Raspberry Pi is a promising candidate for audio processing and this platform is being optimized to take place of a laptop. Another design component is creating a lightweight cane which is properly weighted, with a handle shaped to reduce user fatigue. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 12 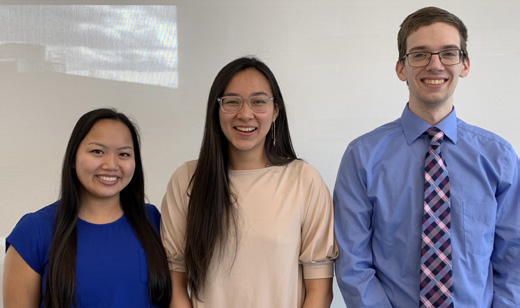 |
Team Ryan McGlynn |
Faculty Advisor(s) Bin Feng, Hugo Posada-Quintero |
Sponsor Biomedical Engineering Sponsor Logo  |
|
|
||||
Description This project proposes the idea of redesigning the conventional thermal grills in order to more effectively simulate pain. The conventional design of the thermal grill consists of pipes pumping hot and cold water alternatively for a sensation of pain upon the subject. The new designs consist of spiral shaped metal and circular focus points with the same alternative pattern but different temperature-regulating mechanisms. Heat will be generated through Joule heating while cooling is stimulated through peltier devices. With the use of the thermal grill illusion, pain will be studied in a more ethical method to further the research of pain measurements. The device aims to provide further data recordings for the discovery of a prominent biosensor when interpreting the pain receptors responding to the sensation of pain. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 13  |
Team Amanda Astrologo |
Faculty Advisor(s) Kristin Morgan |
Sponsor Sport Optimization and Rehabilitation Sponsor Logo  |
|
|
||||
Description Though humans have optimized walking to minimize their energy expenditure, it is still energetically expensive, even for healthy individuals. This naturally poses a further challenge for unhealthy individuals, especially when coupled with unstable walking gait. Thus, our goal is to create an unpowered, adaptive, rehabilitative, medical device that assists in strengthening muscles and promoting self-sufficiency during walking. Our device consists of a belt worn above the hips and a strap sitting below the knee of the affected leg. A rope and elastic band system connected between the hip and the knee utilizes a mechanical pulley-lock mechanism. This mechanism allows the device to control the resistance created by the elastic bands which stretch and relax along the leg as a person walks. The elastic bands store and release energy to relieve the strain in leg muscles, particularly in the hamstrings and quadriceps during walking. From rehabilitating athletes with torn ACLs to assisting the elderly with muscle atrophy, we envision our device to be used for a broad spectrum of patients and for a variety of reasons. Our hope is to contribute to a decreased recovery time for the injured and an increased range of mobility for the weak. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 14  |
Team Brian Chen |
Faculty Advisor(s) Guoan Zheng |
Sponsor UConn School of Nursing Sponsor Logo  |
|
|
||||
Description Individuals with lower back issues suffer chronic pain which can hinder their ability to perform certain tasks. Physical therapy can be a way to subdue the pain, but it can be expensive and requires additional effort to schedule an appointment and leave the home. Yoga can be done at home, but it requires daily effort from the user to remember to practice and performing a pose incorrectly can lead to worsened back pain. Professional yoga will also require additional traveling and fees. The idea behind our senior design project was to create an Android app that avoided these extra fees, traveling, and appointment making with an easy-to-use, free application that allows for pose detection and app usage tracking. These features enable the user to remember to use the app and the poses will be done correctly. Over long periods of practice and app usage, the yoga will help strengthen the user’s back so they can return to their normal life. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 15  |
Team Abdullah Mawla |
Faculty Advisor(s) Guoan Zheng |
Sponsor Biomedical Engineering Sponsor Logo  |
|
|
||||
Description The goal of this project is to develop an inexpensive, easy-to-use Antibiotic Susceptibility Testing (AST) platform for rapid antimicrobial susceptibility profiling of pathogens. This project will utilize Escherichia coli K12 as a model organism. Here we propose a device that incorporates the working principle of light microscopy or a speckle-scanning pictographic lensless imaging scheme to visualize (in real-time) the growth of bacterial cells in a microscopic population throughout an antibiotic concentration gradient. This system will utilize a microfluidic platform that consists of three independent wells connected via a porous membrane to establish the gradient over the middle agar growth well. The device may further be optimized by directly imaging a blood sample, effectively bypassing the time it takes to perform traditional culture isolation and propagation for antibiotic susceptibility testing. The time of AST will be decreased to a 1-2 hour process, with observations of growth taken frequently within this timeframe. A zone of inhibition will be determined using the relative growth of individual cells along the span of the antibiotic gradient. The minimum inhibitory concentration may then be calculated using a linear diffusion approximation. These results will help to conclude what antibiotic is the appropriate treatment for a patient to combat antibiotic resistance. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 16  |
Team Jeremy Bennett |
Faculty Advisor(s) Guoan Zheng |
Sponsor Biomedical Engineering Sponsor Logo  |
|
|
||||
Description We are building a deep-learning powered image classification algorithm that is able to predict the likelihood of glaucoma given a human retina image. Our software utilizes the highly optimized Google image classifier named Inception v3, which has been trained to recognize the presence of multiple common items within an image. Using a training paradigm called transfer learning, we have re-trained the Inception classifier to instead recognize the shapes and patterns that are found in cases of retinal glaucoma. Our software will then be deployed to a website that can be accessed via an app on either an iPhone or Android mobile phone. We hope to show the feasibility of such a clinical decision support system, in which physicians are able to use the prediction of an algorithm that can be retrieved quickly and easily to inform their own decision on patient care. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 17  |
Team Amanda Alkam |
Faculty Advisor(s) Krystyna Gielo-Perczak |
Sponsor Hologic Sponsor Logo  |
|
|
||||
Description The objective of this project was to analyze both physiologic and psychological stress experienced by women during a mammogram. This was done in two ways. First, the standard of care, a flat paddle, was used compared to the stress experienced when SmartCurveTM paddle was used in conjunction with the 3Dimensions Mammography system from Hologic Inc. Second, the participant stood in several different positions similar to those used in a mammogram. The following parameters were measured during the study to quantify the stress response: electromyography (EMG), electrocardiogram (ECG), balance control, Galvanic Skin Response (GSR), and grip strength. A questionnaire was also given to the participant to gain insight on their experience. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 18  |
Team Jordan Daniels |
Faculty Advisor(s) Krystyna Gielo-Perczak |
Sponsor Biomedical Engineering Sponsor Logo  |
|
|
||||
Description Biofeedback is the process of gaining greater awareness of many physiological functions of one's own body, primarily using electronic or other instruments, with a goal of being able to manipulate the body's systems at will. This mind-body technique features the use of visual or auditory feedback to gain control over involuntary bodily functions. The process involves being connected to a device with sensors that provide feedback about specific aspects of your body. The goal of biofeedback is often to make subtle changes to the body that result in a desired effect. This might include relaxing certain muscles slowing heart rate or respiration, or reducing feelings of pain. By doing this, people are often able to improve their physical, emotional, and mental health. The purpose of our study is to reveal instantaneously to patients and therapists certain physiologic events and to teach the patients to control these otherwise involuntary events by manipulating the displayed signals. Results show that biofeedback is applicable to physical rehabilitation through the determination of an optimal recovery method based on a patient’s comfort and muscle activity while performing rehabilitation exercises. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 19  |
Team Avery Carroll |
Faculty Advisor(s) Krystyna Gielo-Perczak |
Sponsor UConn Health Center- The Musculoskeletal Institute Sponsor Logo  |
|
|
||||
Description Reverse Total Shoulder Arthroplasty (rTSA) is becoming a popular surgery to alleviate pain caused by massive rotator cuff damage and shoulder arthritis. However, due to the reversed anatomy, the loads on the muscles within the shoulder are not well known. The Musculoskeletal Institute at UConn Health is currently researching rTSA using a cadaveric shoulder simulator, but the deltoid muscle is not simulated in a way that is accurate to the human anatomy. To shed light on this new anatomy, our team is designing a device that is capable of being installed on the shoulder simulator that will replicate the contraction of the deltoid muscle in the simulator, pulling on both the origin of the deltoid on the acromion, and the insertion of the deltoid on the humerus. The team is involved in the actual trials and testing process which will include data from both native and rTSA implanted shoulders. AnyBody software is also used to model the forces of the deltoid muscle fibers to ensure correct physical modeling. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 20  |
Team Alexander Dowd |
Faculty Advisor(s) Krystyna Gielo-Perczak |
Sponsor Johnson and Johnson: DePuy Synthes Sponsor Logo  |
|
|
||||
Description High ankle sprains are a common injury, specifically amongst collegiate athletes participating in contact sports. This includes the partial or complete tearing of ligaments that makeup the distal tibiofibular syndesmosis, resulting in instability. In some cases, the fibula may fracture at the lateral malleolus or in the diaphysis of the fibula, which is the focus of this project. The current market uses screws and plates to attempt to fixate the tibia, fibula, and talus. Our design focuses on the development of a single use, disposable, sterile surgical kit that allows for non-rigid fixation and stabilization of the distal tibiofibular syndesmosis following a high ankle sprain. The kit will allow for an increased ease of use for the physician, an increased average revenue per case, and will allow for rapid adequate surgical training. The biomechanics of the distal tibiofibular syndesmosis will be investigated, as well as the current products to market, to develop a novel design for Depuy Synthes, part of the Johnson and Johnson medical devices company. Approved through the IRB, human subjects, both healthy and injured, will be analyzed while using the force platform from a sitting to standing position. We will also test our designs in the Depuy Synthes cadaver lab. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 21  |
Team Joemart Ian Contreras |
Faculty Advisor(s) Krystyna Gielo-Perczak |
Sponsor Depuy Synthes Mitek Sports Medicine, a Johnson&Johnson Company Sponsor Logo  |
|
|
||||
Description High ankle sprains are a common injury, specifically amongst collegiate athletes participating in high impact sports such as football, wrestling, and hockey. In the event of a high ankle sprain, the anterior inferior tibiofibular ligament, otherwise known as the AITFL, is partially or completely torn, separating the tibia from the fibula, and leaving the athlete with a long and strenuous recovery. Treatment of the injury depends on the severity, specifically related to whether the fibula fractures and the type of tear. The new designs and techniques being developed will aim to effectively address concerns with current treatment options by providing a comprehensive surgical care kit. The use of surgical tools will further aid in stabilization and healing of the ligaments in situations where more noninvasive treatment options prove unsuccessful. From the information gathered through research, modeling, and testing, the best and most optimal design for treating a high ankle sprain injury with a torn AITFL was determined to consist of using Orthocord suture along with a winged screw to fixate the torn ligament into the posterior end of the bone. An injection of PRP from the patient’s own blood to the site of injury would help expedite the recovery process and prevent chances of chronic ankle instability and post-operative osteoarthritis. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 22  |
Team Maisha Azam |
Faculty Advisor(s) Kazunori Hoshino |
Sponsor Biomedical Engineering Sponsor Logo  |
|
|
||||
Description The group is using in vitro experimentation related to culturing neurons on collagen-filled silk scaffolds in order to most accurately mimic cortical brain tissue and reduce the use of in vivo traumatic brain injury (TBI) testing. Fabricated scaffolds are housed in the constructed incubator, surrounded by the filtration hood, and cultured for extended periods of time under standard cell culture conditions of 5% CO2? and? 37 °C. After the development of sufficient neuronal networks within the scaffolds, the group will perform mechanical trauma experimentation with the force applicator while a high-speed camera records the damage done by the micro-hammer. Displacement along the scaffold can be tracked from multiple video frames. With these results, strain mapping can be completed with correlation to the associated neural network damage. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 23  |
Team Hyuno Chang |
Faculty Advisor(s) Kazunori Hoshino |
Sponsor Biomedical Engineering Sponsor Logo  |
|
|
||||
Description
Hydrocephalus is a condition that affects all populations and results in the buildup of cerebrospinal fluid in the ventricles of the brain. Cerebrospinal fluid (CSF) is fluid produced by the brain through the choroid plexuses that is responsible for protecting the brain and spinal cord, supplying nutrients to nervous system tissue and removing waste products from cerebral metabolism. An excess of CSF in the brain can result in increased intracranial pressure and potentially lead to debilitating symptoms or even death if untreated.
The current standard of treatment for hydrocephalus is to surgically insert a shunt to drain fluid from the ventricles to the abdomen. Approximately 65,000 shunts are implanted each year, and while they are intended to be lifelong implants, they have a 40% malfunction rate within the first two years and a 98% malfunction rate at 10 years, indicating serious problems with current shunt designs. Thus, it is of high interest to develop a shunt sensor capable of monitoring the flow-rate of CSF fluid.
In this project, a novel smart shunt sensor that relies on a PDMS check valve and an optical detection system was successfully fabricated to monitor CSF flow rate. A linear relationship between light intensity and flow rate was found when artificial CSF was pumped through the microfluidic sensor using a syringe pump, proving device capabilities
|
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 24  |
Team Alexis Duggan |
Faculty Advisor(s) Kazunori Hoshino |
Sponsor Biomedical Engineering Sponsor Logo  |
|
|
||||
Description Due to the increasing elderly population and number of complicated bone related diseases, engineers have been investigating the uses of interactive titanium implants in biomedical applications. Current research is still in the process of creating a bioactive and successfully osseointegrated femur implant that is safe to be surgically placed in patients. This report presents possible structures, methods, treatments, and materials that can be implemented to ultimately create a porous, titanium smart implant with microchannels. The implant constructed will have a titanium body with appropriate stiffness, tensile strength, and compressive strength that can be handled in vivo. In addition to this core structure, this implant will also contain a hydrogel scaffold to initiate cell growth and interaction using cell culture and animal cell lines. The hydrogel procedure has been developed and tested, fibroblast cells are being cultured for testing (for future osteoblast use), and these components will combine to form the matrix within the titanium scaffold. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 25  |
Team Nicholas Hartunian |
Faculty Advisor(s) Syam Nukavarapu Ph.D. |
Sponsor Biomedical Engineering Sponsor Logo  |
|
|
||||
Description Decellularization is the process of removing the cells from a tissue, leaving only the extracellular components behind. Biological scaffolds composed of extracellular matrix (ECM) are highly useful for regenerative medicine. Decellularized ECM scaffolds have been shown to induce cell mitogenesis and chemotaxis as well as direct cell differentiation, in ways that non-native scaffolds cannot. The goal of this design experiment was to develop a device that automates a cartilage decellularization protocol. This device enables a researcher to program the desired protocol details, walk away, and return to decellularized tissue. An automated decellularization device presents great promise for tissue engineering research and development, as it streamlines a formerly tedious and potentially inconsistent protocol. The prototype design concept that is proposed consists of seven identical carboys, each connected to a respective solenoid valve with binary fluid control. The bioreactor chamber housing the cartilage will be similar to the carboys; however, it will be equipped with an ultrasonic sensor to monitor fluid levels. The automation of the decellularization protocol will result in a more standardized final tissue scaffold. Moreover, our device will enable the researcher to modify the decellularization protocol much more easily, enabling experimental benefits. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 26  |
Team Joseph Cranston |
Faculty Advisor(s) Ki Chon, Jeffrey Bolkhovsky |
Sponsor Naval Submarine Medical Research Labratory Sponsor Logo  |
|
|
||||
Description Although physical activity is a prominent factor in most people’s daily life, there is little research based on recovery time. The purpose of this study, therefore, was to determine a biometric related to muscle recovery (percent recovered) based on controllable factors. In order to simplify the data, only the biceps were chosen for muscle analysis. The biceps curl was the chosen exercise because it is a simple movement which is easy to perform and monitor. The study was formulated so that an even number of males and females were placed into three test groups. Each group performed the bicep curls on 3 days, the difference between groups being the number of rest days between exercise. Group A had no rest days, group B had one rest day, and group C had 2 rest days. Two forms of data were collected: ECG (electrocardiogram) and EMG (electromyography). ECG sensors were vital in determining participant’s heart rates during resting periods and during exercise, crucial to analyzing heart rate variability. EMG sensors, placed on the participant’s bicep, allowed further analysis of muscle fiber recruitment and intensity over the testing period. The results should show a trend where the subjects with longer time between exercise will have a more active parasympathetic nervous system than those with shorter rest times. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 27  |
Team Tudor Ilies |
Faculty Advisor(s) Bin Feng |
Sponsor Medtronic Sponsor Logo  |
|
|
||||
Description Minimally invasive surgery is a highly advantageous, up and coming field of surgery that limits the number and size of incisions made on the patient, and has proven to be much safer than open surgery. It has been found that adequate local tissue perfusion at the tissue incision site contributes to the success rate of surgical procedures. Being able to identify and quantify local tissue perfusion prior to making an incision would help surgeons operate on the healthiest tissue that is most likely to successfully heal. The goals of this project were to explore various methods of tissue perfusion detection and complete a proof of concept study demonstrating the application of UV-VIS fiber optic spectrometry utilizing two wavelength ranges ( ultra-violet and visible) for local tissue perfusion. A visual representation of local perfusion is shown in Figure 1. The graph shown in Figure 2. is a graph of the unique absorbance peaks of hemoglobin over the utra-violet to visible light wavelength range. |
||||
|
||||
 |
Senior Design 2020 – Biomedical Engineering Team 28  |
Team Denis Caibal |
Faculty Advisor(s) Martin Han |
Sponsor UConn Neural Prostheses Lab Sponsor Logo  |
|
|
||||
Description Parkinson’s disease (PD) is a progressive neurodegenerative disorder that is most easily identified by its impairment of basic motor functions. The highly targeted method of deep brain stimulation (DBS) is an FDA-approved method of treatment for Parkinson’s disease that targets the deep brain’s subthalamic nucleus (STN). DBS delivers electrical stimulation that overrides abnormal electrical signals to decrease the severity of symptoms. This project seeks to make improvements upon 3D printed surgical inserters, used to guide the DBS microelectrodes, to further the accuracy of microelectrode insertions and minimize damage to brain tissue during surgery. Specifically, the improved device will be automated and able to provide real-time data to the user during surgery. The device will need to be highly accurate in order to ensure the microelectrodes reach the STN. The device will be tested on a highly representative brain model using agar to represent the STN and gelatin as the brain tissue. The consistency of gelatin is very similar to brain tissue, provides minimal pathway damage, and is clear, allowing the user to see the insertion as it is occurring. There is both a noticeable difference in consistency between agar and gelatin, as well as an abundance of excess agar that clings to the lead upon removal, allowing the user to easily identify if the STN has been reached. |
||||
|
||||